Osteoporosis
Understanding Osteoporosis: Symptoms, Causes, and Prevention
As you meticulously count the wrinkles appearing on your skin, you might be blissfully unaware that a more pressing concern is your bones’ clandestine escape from robustness. Osteoporosis, a condition you can’t feel or see in a mirror, is quietly compromising the very structure that keeps you upright.
It’s an insidious ailment, often undetected until a fracture occurs, which suddenly and inconveniently reminds you that your body has a few tricks up its sleeve. Now, you’re not made of glass, but understanding how to keep your bones from mimicking its fragility is crucial.
Let’s explore what can be done to strengthen your skeletal system, the consequences of ignoring the silent alarm bells, and why the next steps you take could be the most important in safeguarding your independence and vitality.
Key Takeaways
- Osteoporosis is a condition where bones lose density and strength, increasing the risk of fractures.
- Adequate intake of calcium and vitamin D is essential for maintaining bone density.
- Weight-bearing exercise stimulates bone formation and strengthens skeletal structure.
- Regular check-ups and bone density testing are encouraged for early detection of osteoporosis.
Understanding Osteoporosis

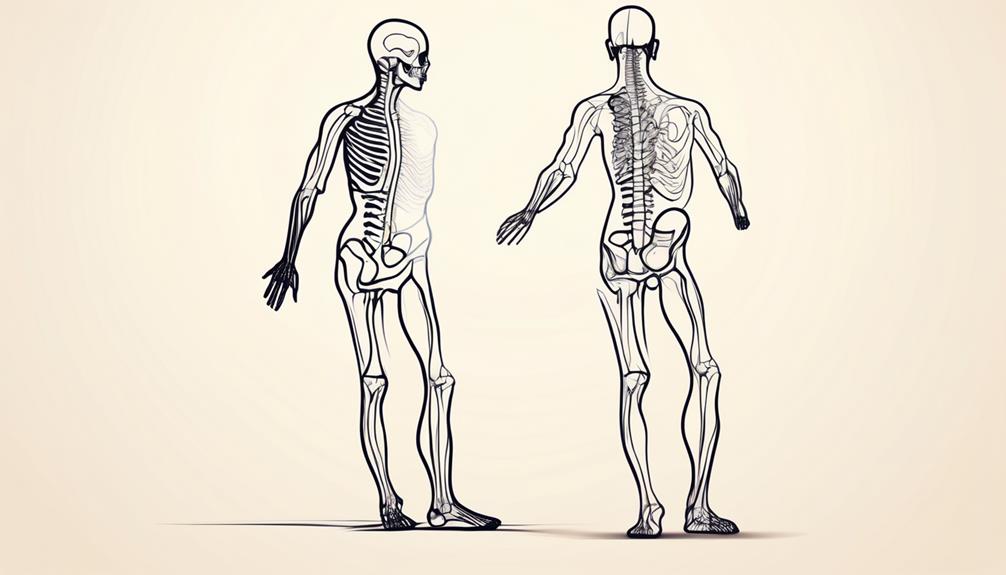
Grasping the complexities of osteoporosis is crucial, as it’s a condition where your bones lose density and strength, significantly increasing the risk of fractures. Your peak bone mass, typically achieved by your late twenties, serves as the foundation for future bone health. Adequate intake of calcium and vitamin D throughout life is essential, as these nutrients are pivotal for maintaining bone density.
In osteoporosis, the microarchitectural integrity of bone tissue deteriorates, leading to an increased susceptibility to fractures, particularly in the hip, wrist, and spine. These fractures can be life-altering, with hip fractures often resulting in a loss of independence and mobility. Osteopenia, a state of reduced bone mass that isn’t quite as severe as osteoporosis, can be a precursor to the condition.
To mitigate bone loss, weight-bearing exercise is recommended, as it stimulates bone formation and strengthens skeletal structure. For individuals at risk, such as postmenopausal women experiencing early menopause, proactive monitoring for signs of bone density reduction is vital. Early intervention and treatment can lessen the progression of osteoporosis and decrease the likelihood of fractures, preserving your ability to serve and care for others effectively.
Identifying Symptoms
Osteoporosis’s subtlety in early stages means you may not notice symptoms until significant bone loss has occurred, often revealed through painful fractures or noticeable changes in posture. As a condition that causes the bones to weaken, understanding the osteoporosis symptoms and causes is pivotal. You mightn’t realize that you or someone you’re caring for has been diagnosed with osteoporosis because many don’t know they’ve osteoporosis until a fracture occurs.
To enhance your ability to serve, consider these signs of osteoporosis:
- A sudden, sharp pain in the back could indicate a spinal fracture.
- A gradual loss of height over time or a stooped posture may signal spinal bone deterioration.
- Unexpected fractures, particularly in the hip or wrist, after minor falls or injuries.
- Frequent complaints of general bone pain or tenderness.
Osteoporosis is often called a silent disease because it can progress undetected. A comprehensive osteoporosis overview includes being vigilant for these symptoms and causes of osteoporosis.
If you’re involved in the care of people with osteoporosis, encourage regular check-ups and bone density testing for early detection. Prompt diagnosis can lead to interventions that may prevent further bone loss and manage the condition more effectively.
Exploring Causes
Delving into the causes of osteoporosis, it’s critical to recognize that both genetic and environmental factors play significant roles in bone density deterioration. Osteoporosis causes bones to become less dense and more prone to fracture. This condition occurs when the creation of new bone doesn’t keep up with the removal of old bone.
Key osteoporosis causes include hormonal imbalances, particularly reduced levels of estrogen in women during menopause and testosterone in men. A family history of osteoporosis can significantly increase one’s risk, indicating a genetic predisposition to the condition.
Furthermore, inadequate intake of calcium and vitamin D, essential for bone mass maintenance, can contribute to the development of osteoporosis. Long-term use of corticosteroid medications, certain cancer treatments, and other drugs that interfere with bone rebuilding can exacerbate bone loss.
Other risk factors are lifestyle choices, such as sedentary behavior, excessive alcohol consumption, and tobacco use. These factors can influence how strong or weak bones become over time.
It’s imperative to understand these mechanisms to effectively serve those at risk or suffering from osteoporosis, optimizing prevention and management strategies to maintain bone health.
Effective Treatments
Understanding the underlying causes of osteoporosis sets the stage for exploring the most effective treatments to manage this bone-weakening disease. As a healthcare professional dedicated to serving others, you’ll find that the management of osteoporosis requires a comprehensive treatment plan, which includes both pharmacological and lifestyle interventions.
Here’s a rundown of the cornerstone elements in osteoporosis treatment:
- Medication: Options such as bisphosphonates, hormone therapy, and denosumab are prescribed to increase bone density and significantly reduce the risk of fractures.
- Supplementation: Ensuring adequate intake of calcium and vitamin D is crucial, and supplementation may be necessary to maintain bone health.
- Exercise: Weight-bearing exercise can help strengthen bones and muscles, and reduce the risk of falls, an important aspect of prevention of osteoporosis.
- Lifestyle Modifications: Encouraging patients to quit smoking and maintain a balanced diet rich in nutrients essential for bone health is part of a holistic treatment approach.
Prevention Strategies
To effectively prevent osteoporosis, it’s essential to regularly engage in weight-bearing and muscle-strengthening exercises that are proven to enhance bone density. By focusing on osteoporosis prevention strategies, you can maintain healthy bone tissue and reduce your risk of falling.
Incorporating regular exercise, particularly diet and weight-bearing exercise, is critical. These activities stimulate bone formation and slow down bone loss. Ensure you’re getting enough calcium through your diet to support bone health. Calcium intake is pivotal, and you should strive to meet the recommended daily amounts specific to your age and gender. Also, vitamin D plays a crucial role in calcium absorption; hence, maintaining adequate levels through sunlight exposure or supplementation is necessary.
Identifying and addressing risk factors for osteoporosis early can greatly diminish the likelihood of developing the condition. Regular bone density testing is recommended for those at higher risk. Here’s a table to guide you in adopting a comprehensive approach:
| Lifestyle Change | Benefit |
|---|---|
| Regular Exercise | Increases bone strength and density |
| Adequate Calcium | Ensures healthy bone maintenance |
| Vitamin D | Facilitates calcium absorption |
| Smoking Cessation | Lowers bone loss and fracture risk |
| Moderation in Alcohol | Preserves bone integrity |
Understanding Osteoporosis: Symptoms, Causes, and Prevention
Osteoporosis is a condition that causes bones to become weak and less dense, increasing the risk of fractures. Many people with osteoporosis don’t know they have it until they experience a fracture or their doctor detects signs through a bone density test.
Symptoms and Causes of Osteoporosis
Osteoporosis often progresses unnoticed until a fracture occurs. Common areas include the spine, wrist, and hip. The development of osteoporosis is often attributed to a lack of calcium and Vitamin D, which are necessary for healthy bone formation. As we age, our bone mass naturally decreases, leading to an increased risk of osteoporosis. Early menopause and certain genetic factors can also increase your risk.
Identifying Risk Factors
Risk factors for osteoporosis include aging, family history, dietary factors, and certain medical conditions. Factors like menopause, long-term steroid use, and insufficient weight-bearing exercise can accelerate bone loss. Know your risk factors to better understand when screening might be necessary.
Preventing Osteoporosis
There are several ways to reduce your risk of developing osteoporosis. Consuming enough calcium throughout your life is vital to maintain peak bone mass. Regular weight-bearing exercise can help to strengthen bones and slow the rate of bone loss, reducing the risk of fractures. Understanding risk factors and working with your healthcare provider can help prevent osteoporosis and maintain healthy bone density.
Osteoporosis Treatment
For those diagnosed with osteoporosis, treatment often focuses on slowing bone loss and preventing fractures. This may involve medication, lifestyle modifications, and a diet containing adequate calcium and vitamin D to support new bone development.
Conclusion
In conclusion, osteoporosis is a silent disease that gradually weakens bones, increasing the risk of fractures. Adequate intake of calcium and vitamin D, along with weight-bearing exercise, are essential for maintaining bone density. Regular check-ups and bone density testing are crucial for early detection. Effective treatments include medication, supplementation, exercise, and lifestyle modifications.
Prevention strategies involve exercise, calcium intake, vitamin D maintenance, and identifying and addressing risk factors. By understanding the symptoms, causes, and prevention of osteoporosis, individuals can take proactive steps to maintain healthy bone density and reduce the risk of fractures.