Rheumatology vs Orthopedic: Exploring the Differences and Benefits
Are you experiencing joint pain or mobility issues? If so, you may be wondering whether to consult a rheumatologist or an orthopedic surgeon. While both specialists deal with musculoskeletal conditions, they have distinct areas of expertise and approaches to treatment. Understanding the differences between rheumatology and orthopedics can help you make an informed decision about which specialist is best suited for your needs.
In this blog post, we will explore the contrasting roles of rheumatologists and orthopedic surgeons, as well as delve into specific health concerns that are commonly addressed by each field. We’ll also examine instances where collaboration between these specialists can offer optimal patient care.
So let’s dive in and discover the benefits of both disciplines when it comes to managing joint pain and other musculoskeletal conditions!
Defining Rheumatology and Orthopedics
Rheumatology and orthopedics are two distinct medical specialties that focus on the musculoskeletal system, but they approach it from different angles. Rheumatology primarily deals with autoimmune diseases and disorders of the joints, muscles, tendons, ligaments, and connective tissues. These conditions can include rheumatoid arthritis, lupus, fibromyalgia, gout, or vasculitis.
On the other hand, orthopedics is a branch of medicine that specializes in diagnosing and treating injuries and ailments affecting the bones, joints (including cartilage), muscles, ligaments and tendons. Orthopedic surgeons often perform surgeries like joint replacements or repairs for fractures. They also deal with sports-related injuries such as torn ligaments or rotator cuff tears.
While both rheumatologists and orthopedic surgeons share an interest in addressing musculoskeletal concerns for their patient’s overall well-being,
their approaches differ significantly. Rheumatologists typically employ non-surgical interventions such as medication management to alleviate pain or reduce inflammation associated with autoimmune diseases.
In contrast, orthopedic surgeons have expertise in surgical interventions when conservative treatments fail to provide relief. They may recommend joint replacement surgery for severe osteoarthritis cases or surgical repair for sports injuries.
Understanding these distinctions between rheumatology and orthopedics is crucial when seeking appropriate care for your specific condition. Whether you require ongoing management of a chronic disease like arthritis or treatment for an acute injury like a fracture,
consulting with either a rheumatologist or an orthopedic surgeon can ensure you receive tailored care based on their specialized knowledge.
Understanding the Health Concerns Addressed by Rheumatologists and Orthopedic Surgeons
When it comes to our musculoskeletal health, both rheumatologists and orthopedic surgeons play important roles in diagnosing and treating various conditions. Rheumatologists specialize in autoimmune disorders that affect the joints, muscles, and bones, such as rheumatoid arthritis or lupus. On the other hand, orthopedic surgeons focus on surgical interventions for injuries and diseases affecting the musculoskeletal system.
Rheumatologists are well-equipped to diagnose and manage chronic conditions like osteoarthritis, gout, or fibromyalgia. They provide non-surgical treatment options including medications, physical therapy recommendations, joint injections with corticosteroids or hyaluronic acid derivatives.
Alternatively, orthopedic surgeons primarily address acute injuries like fractures or torn ligaments requiring surgical intervention. They also handle degenerative conditions like herniated discs or spinal stenosis that may require procedures such as spinal fusion or laminectomy.
While their areas of expertise may differ slightly, both rheumatology and orthopedics aim to improve patient’s quality of life by effectively managing their musculoskeletal health concerns through personalized treatment plans tailored to each individual’s needs.
Roles of Rheumatologists and Orthopedics: A Comparison
Rheumatologists and orthopedic surgeons both play crucial roles in the field of musculoskeletal health, but their areas of focus and expertise differ. Rheumatologists specialize in diagnosing and treating conditions that affect the joints, muscles, and bones, with a particular emphasis on autoimmune diseases such as rheumatoid arthritis. They are experts at managing chronic pain and inflammation associated with these conditions.
On the other hand, orthopedic surgeons primarily deal with surgical interventions for musculoskeletal issues. They specialize in procedures like joint replacements, fracture repairs, and corrective surgeries to treat deformities or injuries affecting the bones and joints. Orthopedic surgeons often work closely with physical therapists to ensure comprehensive rehabilitation after surgery.
While rheumatologists primarily use non-surgical approaches like medication management to treat their patient’s conditions, orthopedic surgeons have extensive training in performing various surgical procedures when conservative treatments fail or are not sufficient.
Collaboration between rheumatologists and orthopedic surgeons is essential in providing comprehensive care for patients. Both specialists bring unique perspectives to the table and can work together to develop personalized treatment plans that address all aspects of a patient’s condition – from medical management to surgical intervention if necessary.
By working collaboratively, these two specialties can provide holistic care that aims not only at eliminating pain but also at improving the quality of life for individuals dealing with complex musculoskeletal issues.
Benefits of Collaboration Between Rheumatologists and Orthopedic Surgeons
Collaboration between rheumatologists and orthopedic surgeons can offer numerous benefits for patients dealing with musculoskeletal issues. These two specialties bring unique perspectives and expertise to the table, allowing for a comprehensive approach to diagnosis, treatment, and management.
One of the key benefits of collaboration is improved accuracy in diagnosing complex conditions. Rheumatologists specialize in autoimmune diseases like rheumatoid arthritis and lupus, while orthopedic surgeons focus on surgical interventions for bone and joint problems. By working together, they can accurately identify the underlying cause of a patient’s symptoms and develop a personalized treatment plan.
Additionally, collaboration ensures that patients receive optimal care throughout their treatment journey. Rheumatologists excel in managing chronic conditions through medication management and lifestyle modifications. Orthopedic surgeons are skilled in performing surgeries such as joint replacements or repairs. When these specialists collaborate, they can provide comprehensive care tailored to each patient’s needs.
Moreover, collaboration promotes better outcomes by minimizing unnecessary treatments or surgeries. Through open communication and shared decision-making, rheumatologists and orthopedic surgeons can determine the most appropriate course of action for each patient. This collaborative approach helps avoid invasive procedures when conservative measures may be more effective.
Furthermore, collaborating allows for ongoing monitoring and follow-up care after surgery or treatment completion. Rheumatologists closely monitor disease activity over time to ensure that medications remain effective or make necessary adjustments if needed. Orthopedic surgeons assess post-operative recovery progress to optimize rehabilitation efforts.
The collaboration between rheumatology and orthopedics offers significant advantages in terms of accurate diagnoses, comprehensive care planning, reducing unnecessary procedures,
and ensuring long-term success through continuous monitoring. By combining their knowledge and skills, these specialists work together to enhance patient outcomes and improve overall quality of life.
Whether it’s addressing chronic conditions like arthritis or providing surgical solutions,
collaboration between rheumatologists and orthopedic surgeons ultimately benefits patients by providing a more holistic and multidisciplinary approach to musculoskeletal
When to Visit an Orthopedic Surgeon
When it comes to musculoskeletal issues, knowing when to visit an orthopedic surgeon is crucial. Orthopedic surgeons specialize in the diagnosis and treatment of conditions affecting the bones, joints, muscles, ligaments, and tendons. If you’re experiencing any of the following symptoms or conditions, it may be time to schedule a consultation with an orthopedic surgeon.
- Persistent joint pain: If you have been dealing with persistent joint pain that doesn’t improve with rest or over-the-counter medications, it’s important to seek medical attention. An orthopedic surgeon can help determine the underlying cause and recommend appropriate treatment options.
- Limited range of motion: Difficulty moving a joint or experiencing stiffness could be indicative of a more serious issue such as arthritis or a ligament tear. An orthopedic surgeon can evaluate your condition and develop a personalized treatment plan.
- Sports injuries: Whether you’ve sustained an injury while playing sports or during physical activity, an orthopedic surgeon is well-equipped to diagnose and treat common sports-related injuries like sprains, fractures, dislocations, and torn ligaments.
- Chronic back pain: Back pain that persists for weeks or months may require specialized care from an orthopedic surgeon who specializes in spine disorders. They can assess your condition through imaging tests like X-rays or MRIs and provide appropriate interventions ranging from conservative treatments to surgical options if necessary.
- Joint instability: If you experience frequent instances where your joints feel unstable or give out unexpectedly (especially in weight-bearing joints like knees), it could indicate ligament damage that requires evaluation by an orthopedic specialist.
Remember that this list is not exhaustive – there are many other scenarios where consulting an orthopedic surgeon would be beneficial for accurate diagnosis and effective management of musculoskeletal conditions.
When to Visit a Rheumatologist
If you’re experiencing persistent joint pain, inflammation, or stiffness that doesn’t seem to go away with rest and over-the-counter medications, it may be time to consider visiting a rheumatologist. Rheumatologists are specialists who diagnose and treat conditions that affect the joints, muscles, bones, and connective tissues.
One common reason to see a rheumatologist is if you have symptoms suggestive of an autoimmune disease. These diseases occur when your immune system mistakenly attacks healthy cells in your body. Conditions like rheumatoid arthritis, lupus, and psoriatic arthritis fall under this category and can cause joint pain, fatigue, swelling, and other systemic symptoms.
Another situation where you might want to consult a rheumatologist is if you’ve been diagnosed with osteoarthritis but are still experiencing significant pain or disability despite conservative treatments like physical therapy or medication adjustments.
Additionally, if you have unexplained musculoskeletal symptoms such as muscle weakness or muscle pain unrelated to injury or exercise, consulting a rheumatologist would be beneficial. They can evaluate whether an underlying inflammatory condition could be causing these symptoms.
It’s also important to consider seeing a rheumatologist if your primary care doctor suspects that your joint issues may not be purely musculoskeletal but rather related to systemic conditions like vasculitis or fibromyalgia.
Overall, a visit with a rheumatologist can provide specialized expertise in diagnosing and managing complex conditions affecting the musculoskeletal system. By partnering with them,
you can receive personalized treatment plans tailored to your specific needs and improve your quality of life. Properly evaluating the possible causes of your symptoms and developing appropriate treatment strategies
How Orthopedic Surgeons and Rheumatologists Approach Shoulder Pain
When it comes to shoulder pain, both orthopedic surgeons and rheumatologists play a crucial role in diagnosing and treating the underlying causes. Orthopedic surgeons are specialized in musculoskeletal conditions and often focus on surgical interventions, while rheumatologists specialize in autoimmune diseases that can affect joints.
Orthopedic surgeons approach shoulder pain by conducting a thorough examination of the affected area. They may order imaging tests such as X-rays or MRI scans to assess any structural abnormalities, such as fractures or tears in the tendons or ligaments. Based on their findings, they may recommend nonsurgical treatments like physical therapy or prescribe medications for pain management.
On the other hand, rheumatologists take a broader perspective when dealing with shoulder pain. They consider not only structural issues but also inflammatory conditions like arthritis that can cause joint discomfort. Rheumatologists will conduct a comprehensive evaluation of your medical history and perform specific blood tests to identify any autoimmune markers or signs of inflammation.
Both specialists work closely together when necessary to provide holistic care for patients experiencing shoulder pain. Collaboration between orthopedic surgeons and rheumatologists ensures an accurate diagnosis and tailored treatment plan based on individual needs.
It’s important to remember that each case is unique, so consulting with either specialist (or both) can help determine which approach is best suited for managing your shoulder pain effectively.
Identifying and Treating Bursitis in the Knees: Rheumatologist vs Orthopedic Surgeon
When it comes to identifying and treating bursitis in the knees, both rheumatologists and orthopedic surgeons play important roles. Bursitis is a condition characterized by inflammation of the bursae, which are small fluid-filled sacs that cushion the joints. It can cause pain, swelling, and limited mobility in the affected area.
Rheumatologists are specialists in diagnosing and managing conditions related to joints, muscles, and connective tissues. They will typically evaluate your symptoms, perform a physical examination, and may order diagnostic tests such as X-rays or MRI scans to confirm the diagnosis of bursitis. Rheumatologists often take a holistic approach to treatment by addressing underlying causes such as arthritis or autoimmune disorders.
On the other hand, orthopedic surgeons specialize in surgical interventions for musculoskeletal conditions like bursitis. If conservative treatments like rest, ice therapy, physical therapy exercises or corticosteroid injections do not provide sufficient relief from knee bursitis symptoms then an orthopedic surgeon might recommend surgery as a last resort option.
Ultimately whether you choose to see a rheumatologist or an orthopedic surgeon for knee bursitis will depend on various factors including your specific symptoms,
medical history, and individual preferences.
Always consult with your primary care physician who can refer you to the appropriate specialist based on their evaluation. Together with either specialty professional, you can develop an individualized treatment plan that suits your needs and helps alleviate your knee pain caused by bursitis
Recovery Time for Knee Replacement Surgery: Insights from Orthopedics and Rheumatology
After undergoing knee replacement surgery, understanding the recovery process is crucial. Both orthopedic surgeons and rheumatologists play important roles in helping patients recover successfully.
Orthopedic surgeons specialize in performing knee replacement surgeries. They are experts in surgical techniques and will guide you through the procedure itself. However, their involvement doesn’t end there. They also provide post-operative care instructions to promote healing and prevent complications.
On the other hand, rheumatologists focus on managing the underlying conditions that contribute to knee pain and joint damage. They can help optimize your overall health before surgery by addressing any inflammation or autoimmune issues that may affect your recovery.
The typical recovery time for knee replacement surgery varies depending on factors such as age, overall health, and adherence to rehabilitation protocols. Generally speaking, it takes several weeks to months for most patients to regain full functionality of their new knee joint.
During this period, a combination of physical therapy sessions, exercises prescribed by both the orthopedic surgeon and rheumatologist (if necessary), pain management strategies, lifestyle modifications (such as weight loss if needed), and follow-up appointments will be essential for a successful recovery.
Remember that each patient’s journey is unique; therefore it is important to consult with both an orthopedic surgeon and a rheumatologist throughout your recovery process so they can tailor treatment plans according to your specific needs.
By working together with these specialists during your rehabilitation period, you’ll have access not only to expertise but also personalized support along every step of your road to recovery after knee replacement surgery
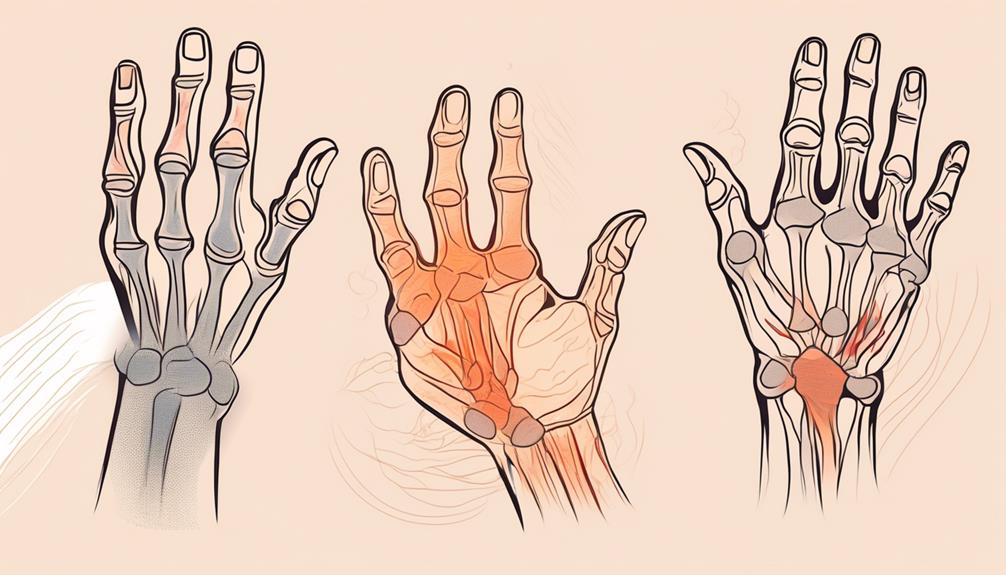
Choosing the Right Specialist for Finger Pain: Rheumatologist or Orthopedic Surgeon?
When it comes to finger pain, determining whether to see a rheumatologist or an orthopedic surgeon can be a challenging decision. Both specialists play important roles in diagnosing and treating various hand and finger conditions.
Rheumatologists are experts in the field of rheumatology, which focuses on arthritis and other autoimmune diseases that affect the joints. They are skilled at identifying and managing inflammatory conditions like rheumatoid arthritis or lupus that may cause finger pain. Rheumatologists often use non-surgical approaches such as medications, physical therapy, and joint injections to alleviate symptoms.
On the other hand, orthopedic surgeons specialize in musculoskeletal disorders and injuries affecting bones, muscles, tendons, ligaments, and joints. They have extensive knowledge of hand anatomy and can diagnose conditions like fractures or tendon injuries that may cause finger pain. Orthopedic surgeons may recommend surgical interventions such as repairing damaged tendons or realigning fractured bones for severe cases.
In some instances when the cause of finger pain is unclear, it might be necessary to consult both specialists for a comprehensive evaluation. This collaborative approach ensures that patients receive personalized care tailored to their specific needs.
Choosing between a rheumatologist or an orthopedic surgeon for finger pain depends on factors such as your medical history, symptoms severity, diagnostic test results if any exist), personal preferences regarding treatment options (surgery vs non-surgical), and input from primary care physicians who will guide you towards the most appropriate specialist based on your unique situation.
Important Questions to Ask During an Appointment with a Rheumatologist or Orthopedic Surgeon
When you have an appointment with a rheumatologist or orthopedic surgeon, it’s important to come prepared with questions that will help you gain a better understanding of your condition and treatment options. Here are some key questions to consider asking during your appointment:
- What is the specific diagnosis for my condition? Understanding the underlying cause of your symptoms can guide treatment decisions and help manage expectations.
- What are the available treatment options? Inquire about conservative approaches (medication, physical therapy) as well as surgical interventions if needed.
- Are there any lifestyle modifications I should make? Ask about exercise recommendations, dietary changes, or other adjustments that may improve your condition.
- What are the potential risks and benefits of each treatment option? It’s crucial to understand both the potential benefits and possible complications associated with different treatments.
- How long will it take for me to see improvements in my symptoms? Getting an idea of the expected timeline for improvement can help set realistic expectations.
- Are there any alternative therapies or complementary treatments worth exploring? Some patients find relief through complementary approaches like acupuncture or chiropractic care – ask if these may be beneficial for you.
- Will I need ongoing follow-up appointments? Understand whether this is a one-time consultation or if regular visits will be necessary for monitoring progress and adjusting treatments if needed.
Remember, these questions serve as starting points – feel free to tailor them based on your specific concerns and needs! Open communication with your healthcare provider is essential in ensuring comprehensive care and making informed decisions regarding your health journey
Understanding Rheumatoid Arthritis and the Best Treatment Approach
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints, causing pain, swelling, and stiffness. It can also impact other parts of the body, such as the heart and lungs. While orthopedic surgeons may be involved in treating joint damage caused by RA, rheumatologists are typically at the forefront of managing this condition.
Rheumatologists play a crucial role in diagnosing and treating RA. They use their expertise to assess symptoms, perform physical examinations, and order imaging tests or blood work to confirm a diagnosis. Once diagnosed with RA, patients usually receive treatment involving medications that reduce inflammation and suppress the immune system.
The best treatment approach for rheumatoid arthritis varies from person to person based on factors like disease severity and individual health status. Rheumatologists often prescribe disease-modifying anti-rheumatic drugs (DMARDs), which slow down joint damage progression. Additionally, they may recommend nonsteroidal anti-inflammatory drugs (NSAIDs) for symptom relief or biological agents targeting specific molecules involved in inflammation.
In some cases where joint damage is severe or unresponsive to medications alone, orthopedic surgeons might come into play. Surgical interventions like joint replacement surgery or synovectomy can help improve function and reduce pain when conservative treatments don’t provide adequate relief.
It’s important to note that while both rheumatologists and orthopedic surgeons can contribute to managing RA effectively, collaborating between these specialists ensures comprehensive care for patients with complex cases requiring surgical intervention alongside ongoing medical management.
Understanding how each specialty contributes its unique expertise towards optimal outcomes for those living with rheumatoid arthritis allows individuals to make informed decisions about their healthcare journey moving forward.
Deciding Between Orthopedics and Rheumatology: Factors to Consider
When it comes to choosing between orthopedics and rheumatology for your healthcare needs, there are several factors that you should consider. Both specialties focus on musculoskeletal health, but they approach it from different angles.
Consider the nature of your condition or concern. Orthopedic surgeons primarily deal with injuries and conditions affecting the bones, joints, muscles, ligaments, and tendons. If you have a broken bone or torn ligament due to an accident or sports injury, an orthopedic surgeon would be the appropriate choice.
On the other hand, if you’re experiencing chronic joint pain or inflammation without any obvious physical trauma, a rheumatologist may be more suitable. Rheumatologists specialize in autoimmune diseases and disorders such as rheumatoid arthritis and lupus which can cause joint pain and swelling.
Another factor to consider is the treatment options available in each specialty. While both orthopedists and rheumatologists can prescribe medications for pain relief and inflammation control, their approaches differ when it comes to surgical interventions.
Orthopedic surgeons are trained in performing surgeries such as joint replacements or repairs for fractures. If surgery is likely required for your condition’s management or improvement, such as severe osteoarthritis, consulting with an orthopedist makes sense.
However, if surgery isn’t necessary at this time or if your condition falls within the realm of non-surgical treatments like physical therapy or medication adjustments based on blood tests (common in certain autoimmune conditions), then consulting with a rheumatologist might be more appropriate.
Furthermore; take into account your personal preferences when deciding between these two specialties. Do you prefer a more conservative approach before considering surgery? Are you interested in exploring alternative therapies like acupuncture? These preferences will play a role in determining which specialist best aligns with your values and beliefs about healthcare.
Conclusion: finding the best fit for your needs.
Rheumatologists treat joint, muscle, and bone conditions without apparent injuries, focusing on autoimmune diseases like rheumatoid arthritis. Orthopedic surgeons handle musculoskeletal injuries, surgeries for fractures, and degenerative issues like osteoarthritis, offering surgical and rehabilitation solutions.
Collaboration between both specialists enhances patient care, combining their expertise for a holistic approach. Patients should discuss symptoms, diagnosis methods, treatment options, and recovery plans with their doctors to make informed decisions.
Choosing between a rheumatologist or orthopedic surgeon depends on the nature of your condition, but consulting both may offer a more comprehensive understanding and treatment plan.