Understanding Gout Rheumatology: Causes, Symptoms, and Treatment Options
Are you experiencing excruciating pain, swelling, and stiffness in your joints? If so, you may be familiar with the debilitating condition known as gout. Gout rheumatology is a specialized field that focuses on understanding and treating this painful form of arthritis.
Whether you’re seeking answers for yourself or someone you care about, this blog post will provide valuable insights into the causes, symptoms, and treatment options for gout. So sit back, relax, and let’s dive into the world of gout rheumatology to help shed light on this often misunderstood condition!
What is Gout?
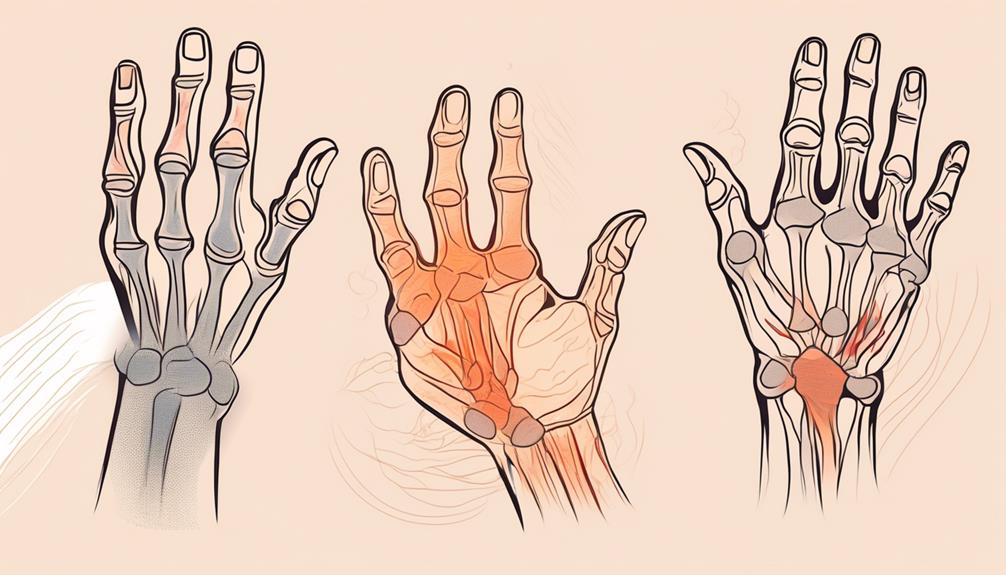
Gout is a form of arthritis that can cause excruciating pain and discomfort. It occurs when there is an excess buildup of uric acid in the body, leading to the formation of sharp crystals in the joints. This condition primarily affects the big toe, but it can also affect other joints such as the ankles, knees, wrists, and elbows.
Understanding Gout Rheumatology
The exact cause of gout is still unknown, but it is believed to be a result of a combination of genetic factors and lifestyle choices. Certain foods high in purines, such as red meat and seafood, can trigger gout attacks. Other risk factors include obesity, excessive alcohol consumption, high blood pressure, and certain medical conditions like diabetes and kidney disease.
The clinical presentation of gout typically involves sudden onset joint pain accompanied by swelling and inflammation. These flare-ups can last for several days or weeks before subsiding on their own. Diagnosis usually involves a physical examination along with blood tests to measure uric acid levels in the body.
There are various treatment options available for managing gout. During acute flare-ups, medications like nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to alleviate pain and reduce inflammation. Urate-lowering therapies are used to prevent future attacks by lowering uric acid levels in the body.
In addition to medication management, lifestyle modifications play a crucial role in controlling gout symptoms. Avoiding trigger foods rich in purines like organ meats and shellfish can help decrease the frequency of flare-ups. Maintaining a healthy weight through regular exercise and following a balanced diet low in saturated fats can also contribute positively towards managing this condition.
Living with gout can be challenging both physically and mentally. The chronic nature of this condition often leads to feelings of frustration or isolation for individuals affected by it; hence support networks are essential for coping with these challenges effectively.
The stigma surrounding gout can also affect mental health, making it important to raise awareness and promote understanding
Definition and Overview
Gout, a type of inflammatory arthritis, is often referred to as “the disease of kings.” But don’t let the regal nickname fool you – gout can affect anyone. It is caused by high levels of uric acid in the blood, leading to the formation of needle-like crystals in joints and surrounding tissues. These crystals cause sudden and severe joint pain, which is typically accompanied by redness, swelling, and heat.
When it comes to understanding gout rheumatology, it’s essential to recognize that this condition primarily affects the big toe joint. However, it can also impact other joints such as ankles, knees, elbows, wrists or fingers. The onset of symptoms can be rapid and unexpected—often occurring during sleep or after a period of intense physical activity or excessive alcohol consumption.
Gout is not merely a passing discomfort; it can significantly impact an individual’s quality of life if left untreated. Recurrent flare-ups may lead to chronic inflammation and damage to joints over time. Therefore early diagnosis becomes crucial for effective management.
To accurately diagnose gout rheumatology specialists rely on several factors including medical history evaluation along with physical examination findings such as tenderness at affected joints.
A definitive diagnosis is made through fluid aspiration from an inflamed joint followed by analysis under polarized light microscopy, a technique that reveals the presence of characteristic urate crystals.
Causes of Gout
Gout, a form of arthritis, is primarily caused by the buildup of uric acid crystals in the joints. But what exactly leads to this accumulation? Well, it all starts with purines – compounds found naturally in certain foods and our body’s cells.
When we consume purine-rich foods such as red meat, seafood, and alcohol (especially beer), our bodies break down these purines into uric acid. Normally, uric acid dissolves in the blood and gets eliminated through urine. However, when there’s an excessive production or inadequate excretion of uric acid, it can lead to its deposition in the joints.
- Several factors contribute to increased levels of uric acid. Genetics play a role too – if you have family members with gout or hyperuricemia (high levels of uric acid), your risk increases significantly.
- Other lifestyle choices also impact your susceptibility to gout. Obesity and a diet high in processed sugars raise your chances of developing this condition. Additionally, medical conditions like hypertension and kidney disease can disrupt normal urate metabolism and trigger gout attacks.
Understanding the causes behind gout enables individuals to make informed decisions about their lifestyles and dietary choices that may reduce their risk or prevent flare-ups from occurring. By adopting healthier habits and managing underlying conditions effectively, one can actively take control over their health journey!
Risk Factors
Gout is a complex condition that can be influenced by various risk factors. While it primarily affects men over the age of 40, women and younger individuals can also develop this painful form of arthritis. One of the most significant risk factors for gout is diet. Consuming foods high in purines, such as red meat, seafood, and alcohol, can increase uric acid levels in the body and contribute to gout attacks.
- Genetics also play a role in determining an individual’s susceptibility to gout. If you have a family history of gout or kidney disease, you may be at higher risk for developing this condition. Other medical conditions like obesity, hypertension (high blood pressure), diabetes mellitus type 2, and metabolic syndrome are also known to increase the likelihood of experiencing gout flare-ups.
- Certain medications can also increase your chances of developing gout. Diuretics used to treat high blood pressure and heart failure can elevate uric acid levels in the body if not properly managed with medication adjustments or lifestyle changes.
- It’s important to note that lifestyle choices can greatly impact your risk of developing gout. Maintaining a healthy weight through regular exercise and following a balanced diet low in purine-rich foods may help reduce your likelihood of experiencing painful flare-ups.
While these risk factors don’t guarantee that you will develop gout, being aware of them allows you to make informed decisions about managing your health and reducing potential triggers for flare-ups. Speak with your healthcare provider about any concerns or questions regarding your risk factors for gout.
Clinical Presentation of Gout
Gout, a form of inflammatory arthritis, is known for its sudden and intense attacks of pain. The affected joint becomes red, swollen, and extremely tender to the touch. These flare-ups typically occur in the big toe but can also affect other joints such as the ankle, knee, or wrist.
- During an acute gout attack, individuals often experience excruciating pain that peaks within 24 hours and slowly subsides over several days. The affected joint may feel hot to the touch due to inflammation. Even simple activities like walking or wearing shoes can become unbearable.
- In addition to severe pain and swelling, people with gout may also experience other symptoms such as fever and fatigue during an attack. Some individuals may even develop a low-grade fever alongside their joint symptoms.
- It’s important to note that not all cases of gout present with these classic symptoms. Some individuals may only have mild discomfort without significant swelling or redness during an episode.
- Diagnosing gout requires careful evaluation by a healthcare professional who will consider various factors including symptom presentation, medical history, physical examination findings (such as joint tenderness), and laboratory tests (like elevated levels of uric acid).
Early recognition and diagnosis are crucial for effective management of this condition. If you suspect you might be experiencing gout symptoms, it’s essential to seek medical attention promptly for appropriate evaluation and treatment options tailored specifically to your needs.
Signs and Symptoms
Signs and symptoms of gout can vary from person to person, but they typically manifest in the form of sudden and intense joint pain. The most commonly affected joint is the big toe, although gout can also affect other joints such as the ankles, knees, elbows, wrists, and fingers.
- During a gout attack, individuals may experience redness and swelling around the affected joint. The area may feel hot to the touch and be extremely tender. Even light pressure or movement can cause excruciating pain.
- In addition to joint inflammation, some people with gout may develop small lumps under their skin called tophi. Tophi are deposits of urate crystals that accumulate over time due to high levels of uric acid in the body. These lumps are usually painless unless they become inflamed or infected.
- Gout attacks often occur suddenly without warning signs or specific triggers. They tend to peak within 24-48 hours before gradually subsiding over several days or weeks. However, it’s important to note that not everyone with elevated uric acid levels will experience these acute flare-ups.
If you experience any of these symptoms or suspect you might have gout, it’s crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options tailored specifically for you.
Diagnosis of Gout
One of the key aspects of understanding gout rheumatology is diagnosing this condition accurately. Gout can often be mistaken for other conditions due to its similar symptoms, so a proper diagnosis is crucial.
- To diagnose gout, healthcare professionals typically start with a detailed medical history and physical examination. They may ask about your symptoms, family history of gout or other related conditions, and any medications you are currently taking. During the physical exam, they will look for signs such as joint inflammation and tenderness.
- In addition to these initial steps, doctors may also use various diagnostic tests to confirm the presence of gout. One common test is the joint fluid analysis. A small amount of fluid is extracted from an affected joint using a needle and then examined under a microscope for urate crystals.
- Blood tests are another tool used in diagnosing gout. These tests measure levels of uric acid in your blood. Elevated levels can indicate the presence of gout or other conditions that cause high uric acid levels.
- Imaging studies like X-rays or ultrasounds may also be used to assess joint damage caused by chronic gout.
Remember, accurate diagnosis is essential for effective treatment planning and management of gout rheumatology! Always consult with a healthcare professional if you suspect you have this condition.
Treatment Options for Gout
Treatment options for gout revolve around managing acute flare-ups and reducing uric acid levels in the body to prevent future attacks.
- Acute Flare-up Management: During a gout attack, the focus is on relieving pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, are commonly prescribed to reduce swelling and discomfort. Colchicine may also be used to alleviate symptoms.
- Urate-Lowering Therapies: To address the underlying cause of gout, medications like allopurinol or febuxostat are prescribed to lower uric acid levels in the blood over time. These medications work by inhibiting an enzyme involved in uric acid production.
- Concurrent Medications and Lifestyle Modifications: Along with medication, doctors often recommend lifestyle changes to manage gout effectively. This includes maintaining a healthy weight, avoiding purine-rich foods (e.g., organ meats, and shellfish), limiting alcohol consumption, staying hydrated, and exercising regularly.
By following these treatment strategies, individuals with gout can experience reduced frequency and severity of flare-ups while improving their overall quality of life.
Acute Flare-up Management
Acute flare-ups of gout can be incredibly painful and debilitating, often leaving individuals searching for immediate relief. Managing these episodes is crucial not only to alleviate the discomfort but also to prevent long-term joint damage.
- One of the first steps in acute flare-up management is pain control. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce inflammation and provide relief. Colchicine, a medication specifically used for gout flares, may also be recommended.
- In addition to medications, lifestyle modifications can play a significant role in managing acute flare-ups. Applying ice packs to the affected joints can help reduce swelling and soothe pain. Resting the joint and elevating it whenever possible can aid in alleviating pressure.
- It’s important to stay hydrated during a flare-up as well since dehydration can worsen symptoms. Avoiding trigger foods such as red meat, seafood, alcohol, and sugary beverages may help prevent future attacks.
Remember that prompt treatment during an acute episode is essential for faster recovery and enhanced quality of life. Always consult with your healthcare provider for personalized advice tailored specifically to your condition.
Urate-Lowering Therapies
Urate-lowering therapies are an essential component in the management of gout. These medications work by reducing the levels of uric acid in the body, which helps to prevent future flare-ups and long-term joint damage.
- One commonly prescribed type of urate-lowering therapy is allopurinol. This medication works by inhibiting an enzyme called xanthine oxidase, which is responsible for the production of uric acid. By blocking this enzyme, allopurinol effectively lowers uric acid levels in the blood.
- Another option for urate-lowering therapy is febuxostat. Similar to allopurinol, febuxostat also inhibits xanthine oxidase and reduces uric acid production. It is effective in lowering serum urate levels and preventing gout attacks.
- In some cases, if patients cannot tolerate or do not respond adequately to these medications, other options may include probenecid or pegloticase. Probenecid works by increasing the excretion of uric acid from the body through urine, while pegloticase is an intravenous medication that breaks down excess uric acid.
- It’s important to note that starting a new medication can sometimes cause a temporary increase in gout flares as old crystals dissolve and new ones form. However, with consistent adherence to treatment and regular monitoring by a healthcare professional, patients can experience significant improvement in their symptoms over time.
Remember, it’s crucial to consult with your rheumatologist or healthcare provider before starting any new medications or making changes to your current treatment plan. They will assess your individual needs and provide personalized recommendations based on your specific situation.
Concurrent Medications and Lifestyle Modifications
When it comes to managing gout, medications and lifestyle changes go hand in hand. Along with prescribed medications, making certain modifications to your daily routine can greatly help reduce the frequency and severity of gout flare-ups.
- One common medication used for gout is nonsteroidal anti-inflammatory drugs (NSAIDs). These drugs help relieve pain and reduce inflammation during acute flare-ups. Another option is colchicine, which can be taken as a preventive measure or during an attack to alleviate symptoms.
- In addition to the right medication, lifestyle modifications play a crucial role in managing gout. One key aspect is maintaining a healthy weight through regular exercise and a balanced diet. Shedding those extra pounds not only reduces the strain on your joints but also helps lower uric acid levels in the body.
- Speaking of diet, avoiding foods high in purines such as red meat, shellfish, organ meats, and alcohol can significantly decrease uric acid production. Opting for low-purine alternatives like fruits, vegetables, whole grains, and lean proteins can have a positive impact on your overall health as well.
- Hydration cannot be stressed enough when it comes to preventing gout attacks. Drinking plenty of water helps flush out excess uric acid from your system and keeps you properly hydrated.
It’s important to remember that these concurrent medications and lifestyle modifications are long-term solutions rather than quick fixes. Actively incorporating them into your everyday life alongside appropriate medical treatment under the guidance of healthcare professionals specialized in rheumatology or related fields will provide you with better control over this painful condition.
Living with Gout
Living with gout can be challenging, but with the right strategies and support, you can effectively manage this condition and improve your quality of life. One key aspect of managing gout is making lifestyle modifications. This includes adopting a healthy diet that is low in purines, which are found in certain foods such as red meat and seafood.
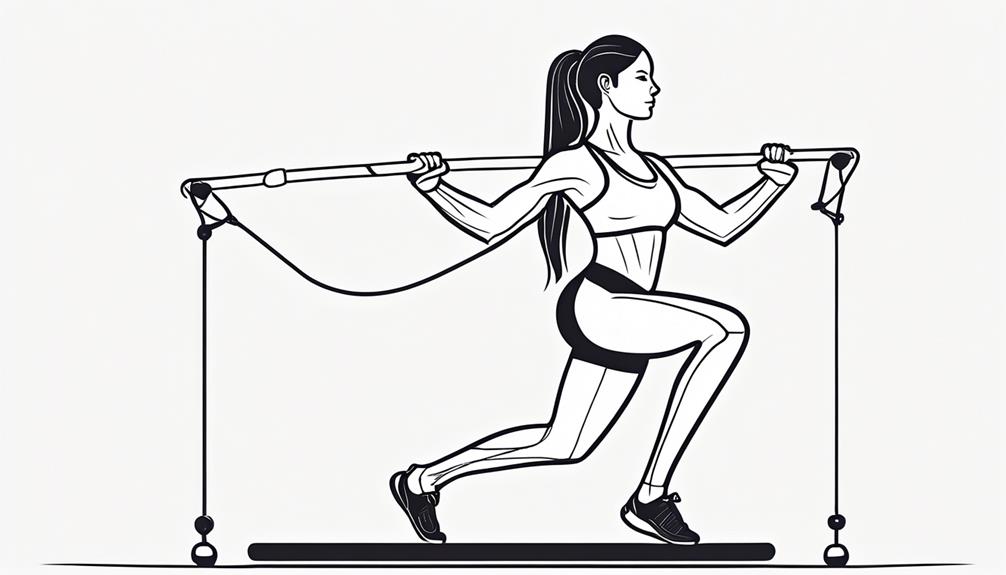
- Regular exercise is also important for maintaining a healthy weight and reducing the risk of gout flares. However, it’s crucial to choose activities that are gentle on the joints to avoid triggering pain or inflammation.
- Managing stress levels is another important aspect of living with gout. High stress levels have been associated with an increased frequency of gout attacks. Finding relaxation techniques that work for you, such as meditation or yoga, can help reduce stress and potentially prevent flare-ups.
- In addition to these lifestyle changes, it’s essential to adhere to any prescribed medications for gout management. Urate-lowering therapies are commonly used to decrease uric acid levels in the body and prevent future flare-ups.
- It’s worth noting that living with gout may also involve dealing with the stigma surrounding this condition. Despite its prevalence, there can still be misunderstandings about what causes gout or how it should be managed. This lack of understanding may lead some individuals to feel embarrassed or isolated due to their diagnosis.
- Addressing mental health concerns related to living with chronic conditions like gout is equally important. Seeking support from friends, and family members, or joining supportive networks and associations dedicated specifically to those managing arthritis-related conditions can provide valuable emotional support during difficult times.
Remember that everyone’s experience with gout will differ based on factors like severity and personal circumstances.
However, by implementing appropriate treatment strategies along with positive lifestyle changes such as dietary adjustments and stress reduction techniques. it becomes possible not only to achieve symptom relief but also to enhance overall well-being while living successfully despite this condition
Managing Gout and Improving Quality of Life
Living with gout can be challenging, but there are steps you can take to manage the condition and improve your quality of life. The key is to adopt a holistic approach that incorporates both medical interventions and lifestyle modifications.
- It’s important to work closely with your healthcare team to develop an individualized treatment plan. This may include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to manage acute flare-ups and prevent future attacks.
- In addition to medication, lifestyle changes play a crucial role in managing gout. Maintaining a healthy weight through regular exercise and a balanced diet low in purines (found in foods like red meat, seafood, and alcohol) can help reduce uric acid levels in the body.
- Staying hydrated is also essential for flushing out excess uric acid from the system. Aim for at least eight glasses of water per day and limit sugary beverages that can contribute to weight gain.
- Furthermore, avoiding triggers such as certain foods or intense physical activity during flare-ups can help prevent further inflammation and pain. Taking time for self-care activities like relaxation exercises or stress management techniques can also provide relief from symptoms.
- Seeking support from others who understand what you’re going through can make a significant difference in managing gout. Joining support groups or online communities allows you to share experiences, exchange tips on coping strategies, and find emotional support during challenging times.
Remember that everyone’s journey with gout is unique – what works for one person might not work for another. By taking proactive steps towards managing your condition while nurturing overall well-being, you’ll be better equipped to lead a fulfilling life despite having gout.
Stigma and Mental Health
Living with gout can be a challenging experience, not only due to the physical symptoms but also because of the potential stigma that may come with it. Unfortunately, gout is often misunderstood and unfairly associated with negative stereotypes. This can have a significant impact on an individual’s mental health and overall well-being.
- One common misconception about gout is that it is solely caused by poor lifestyle choices or overindulgence in certain foods and alcohol. This belief can lead to blame being placed on individuals who have gout, resulting in feelings of shame and self-judgment. It’s important to remember that gout is a complex medical condition influenced by multiple factors such as genetics, age, gender, and underlying health conditions.
- The stigma surrounding gout can also affect interpersonal relationships. People with gout may feel embarrassed or hesitant to discuss their condition openly for fear of judgment or ridicule. This can lead to social isolation and feelings of loneliness, which can further exacerbate mental health issues.
- Additionally, living with chronic pain from recurrent flare-ups may take a toll on one’s emotional well-being. Gout attacks are incredibly painful and unpredictable, making it difficult for individuals to engage in daily activities or maintain their usual level of productivity. The constant worry about when the next attack will occur can contribute to anxiety and stress.
Healthcare professionals and society as a whole must challenge these stigmas associated with gout rheumatology. By promoting education and understanding the true causes of this condition, we can help reduce the burden faced by those living with gout.
Supportive networks play an essential role in combating stigma related to gout rheumatology. Connecting with others who share similar experiences through support groups or online communities can provide valuable emotional support while reducing the sense of isolation often experienced by individuals affected by this condition.
Furthermore, individuals living with gout need to prioritize their mental well-being alongside their physical health. Seeking professional help from therapists or counsellors can be beneficial in managing emotional
Clinical Tools and Guidelines for Gout Rheumatology
When it comes to managing gout, healthcare professionals rely on clinical tools and guidelines to provide the best possible care for their patients. These resources help guide diagnosis, treatment decisions, and overall management of this complex condition.
- One crucial resource in gout rheumatology is the use of clinical practice guidelines. These evidence-based recommendations are developed by expert panels who review current research and provide guidance on various aspects of gout management. They cover topics such as diagnosing gout, assessing disease severity, initiating treatment, and monitoring patient progress.
- In addition to guidelines, there are also valuable clinical tools available to aid healthcare providers in the evaluation and management of gout. These tools can include diagnostic algorithms or flowcharts that assist in diagnosing gout based on symptoms, physical examination findings, laboratory tests (such as serum urate levels), or imaging studies (like ultrasound).
- Another important aspect of managing gout is understanding the criteria used for diagnosis. The American College of Rheumatology has established specific criteria that consider a combination of clinical features and laboratory results to confirm a diagnosis of gout accurately.
It’s essential for healthcare professionals involved in treating individuals with gout to stay updated with the latest research findings and advancements in this field. By utilizing these clinical tools and following evidence-based guidelines, they can ensure optimal care delivery for their patients.
Remember that finding a specialist experienced in managing gout is crucial for obtaining accurate diagnoses and personalized treatment plans. Additionally, supportive networks like patient associations can offer valuable resources both for patients seeking information about their condition and healthcare professionals looking to enhance their knowledge base.
Combining these clinical tools with ongoing education efforts focused on improving outcomes for those living with gout rheumatology conditions can continue evolving positively over time.
Clinical Practice Guidelines
Clinical practice guidelines are evidence-based recommendations that guide healthcare practitioners in delivering optimal care to patients with gout rheumatology. These guidelines are developed by expert panels composed of healthcare professionals and researchers who review the available scientific literature.
The primary goal of clinical practice guidelines is to standardize the diagnosis, treatment, and management of gout across different healthcare settings. They provide a framework for healthcare providers to make informed decisions based on the best available evidence.
These guidelines cover various aspects of gout management, including acute flare-up management, urate-lowering therapies, and concurrent medications and lifestyle modifications. They outline specific recommendations regarding drug selection and dosing, as well as monitoring parameters for assessing treatment response and potential adverse effects.
By adhering to these guidelines, healthcare practitioners can ensure consistent and high-quality care for individuals with gout rheumatology. However, it is important to note that clinical judgment should be exercised when applying these recommendations as patient preferences and individual circumstances may vary.
Healthcare professionals involved in the management of gout rheumatology need to stay updated with current clinical practice guidelines. Regularly reviewing these guidelines helps ensure that patients receive the most effective treatments based on the latest research findings.
In addition to guiding clinicians, clinical practice guidelines also serve as valuable resources for patients seeking information about their condition. Patients can use these guidelines to understand recommended treatment approaches, potential side effects of medications used in gout therapy, and strategies for managing flares or preventing future attacks.
Awareness and implementation of clinical practice guidelines contribute significantly towards improving patient outcomes in gout rheumatology. Healthcare providers should collaborate closely with their patients while considering individual needs when applying these evidence-based recommendations in real-world practice settings.
Clinical Tools and Resources for Gout Rheumatology
When it comes to managing gout, healthcare professionals rely on various clinical tools and resources to guide their treatment decisions. These tools are designed to assist in the diagnosis, assessment, and monitoring of patients with gout.
One essential resource is the clinical practice guidelines for gout rheumatology. These guidelines provide evidence-based recommendations on best practices for diagnosing and treating gout. They help ensure that healthcare providers stay up-to-date with the latest research findings and deliver optimal care to their patients.
In addition to guidelines, there are also specific clinical tools available that aid in the diagnosis of gout. For example, imaging techniques such as ultrasound or dual-energy computed tomography (DECT) can be used to visualize urate crystals in affected joints, confirming a diagnosis of gout.
Furthermore, certain criteria have been established to support accurate diagnostic classification of gout. The most commonly used criteria include those developed by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR). These criteria consider factors such as symptoms, laboratory test results, joint involvement patterns, and response to treatment when assessing whether an individual has gout.
To complement these tools and criteria, there are also numerous online resources available for both healthcare professionals and patients alike. Websites like the Arthritis Foundation or professional organizations like the American College of Rheumatology offer valuable information about managing this condition effectively.
By utilizing these clinical tools and resources effectively in daily practice, the management of patients with gout can be optimized, and they can experience improved outcomes overall.
Criteria for Diagnosis
Diagnosing gout can be a complex process, as the symptoms can mimic other conditions. However, there are certain criteria that doctors use to make an accurate diagnosis. These criteria include clinical features and laboratory tests.
Clinical features play a crucial role in diagnosing gout rheumatology. The characteristic symptom of gout is intense pain and swelling in the joints, typically affecting the big toe. Other affected joints may include the ankles, knees, elbows, wrists or fingers. The pain often starts suddenly and may be accompanied by redness and warmth around the joint.
Laboratory tests are also essential for confirming a diagnosis of gout rheumatology. One common test is examining synovial fluid from an affected joint under a microscope to look for urate crystals. Elevated levels of serum uric acid in blood tests also support the diagnosis.
To meet the diagnostic criteria for gout rheumatology established by organizations like the American College of Rheumatology (ACR), one must have both clinical evidence (such as recurrent episodes of acute arthritis) and at least one positive laboratory finding (such as the presence of urate crystals).
It’s important to note that accurate diagnosis is vital to ensure appropriate treatment strategies are implemented promptly. If you suspect you may have gout rheumatology based on your symptoms, it’s essential to consult with a healthcare professional who specializes in this condition.
Remember, early detection and intervention can help manage symptoms effectively and prevent long-term complications associated with untreated gout rheumatology
Conclusion
In this blog post, we have explored the world of gout rheumatology, delving into its causes, symptoms, and treatment options. Gout is a complex condition that affects many individuals worldwide. By understanding its underlying mechanisms and risk factors, we can better manage and prevent flare-ups.
Managing gout involves a multifaceted approach. Acute flare-ups require immediate attention to alleviate pain and inflammation. Urate-lowering therapies are essential for long-term management by reducing uric acid levels in the body. Concurrent medications and lifestyle modifications play a crucial role in maintaining overall health.
Living with gout can be challenging but not impossible. It’s important to adopt healthy habits such as maintaining a balanced diet, regular exercise routine, staying hydrated, managing stress levels, and getting adequate sleep.
When it comes to resources for gout rheumatology, there are various clinical tools available for healthcare professionals to aid in diagnosis and treatment decisions. Clinical practice guidelines provide evidence-based recommendations to guide medical practitioners in their practice.
If you or someone you know is dealing with gout or suspects having this condition due to persistent joint pain or swelling, it is advisable to seek help from a specialist who has expertise in rheumatology. They will be able to offer personalized care based on your specific needs.
Supportive networks and associations exist where patients can find solace by connecting with others who share similar experiences through online forums or support groups offline.
Remember that knowledge is power when it comes to managing any health condition like gout or rheumatology.